Protecting High-Risk Individuals Means Considering the Economic Cost of COVID-19
June 28, 2022
By Julia Raifman, Aaron Sojourner
As the COVID-19 pandemic continues, evaluating who is bearing continuing health and economic costs is key to informing policy decisions. Protecting people who are elderly, immunocompromised, or have other health conditions has rightly been a priority due to their increased vulnerability to severe COVID-19 outcomes. However, low-income populations and Black, Hispanic,¹ and Native American communities who have elevated risks of exposure, infection, and severe disease due to occupational segregation and more crowded housing have not been given the same prioritization.
In this analysis, we document disparities in missed work due to COVID-19 by income, race, ethnicity, and education level based on nationally representative Household Pulse Survey (HPS) data from Americans aged 18 to 64 years, collected between August 2020 and June 2022. Economic hardship, food insufficiency, and housing insecurity can yield lifelong ramifications for health, human capital, and well-being for already marginalized communities, increasing current levels of economic insecurity and decisively dampening their long-term capacity to move out of poverty. Moreover, the costs of such inequality spill over to the broader economy, leading to service and supply chain disruptions.
The risks and burden of COVID-19 are larger for marginalized populations.
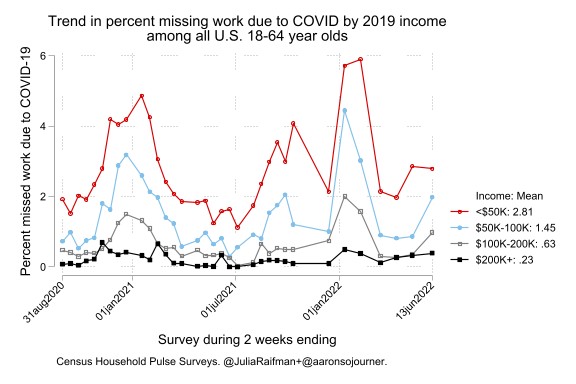
The HPS analysis shows that low-income Americans were the first to report missing work and experienced the most loss of work during COVID-19 case surges, consistent with high exposure to the virus through work, household crowding, and community. Additionally, the burden of COVID-19 cases and missed work is high and much more severe for Black, brown, and low-income households. Prior analysis shows that beyond the acute and long-term health risks of COVID-19, disruptions in income and schedule caused by missed work lead workers to face severe food insufficiency, especially in the absence of paid sick leave. Lower-income workers are much less likely to have paid sick leave, which would offer material help to their families during times of lost income, even though they are the ones who need it most. These compounding factors significantly increase marginalized communities’ health and economic risks.
Low-income and other marginalized groups face higher levels of exposure to COVID-19.
The new HPS analyses show that Americans in families earning less than $50,000 in 2019 were 12 times more likely to report missing a full week of work due to COVID-19 than those earning at least $200,000.
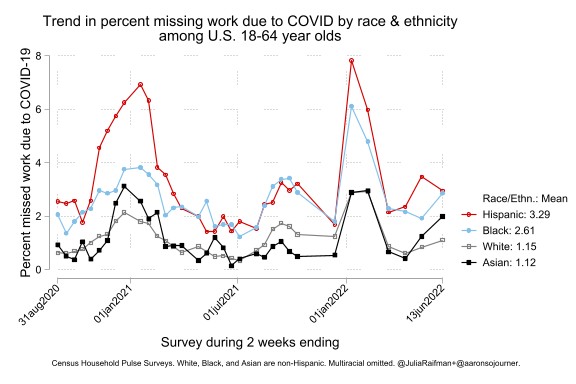
This new analysis also finds persistent racial and ethnic disparities, which widened early and persisted over time. Across this period, Hispanic and Black Americans were more than twice as likely to report missing work due to COVID-19 symptoms as white or Asian Americans. This finding is consistent with CDC data showing that Black, Hispanic, and Native American people have been more likely to contract and die of COVID.
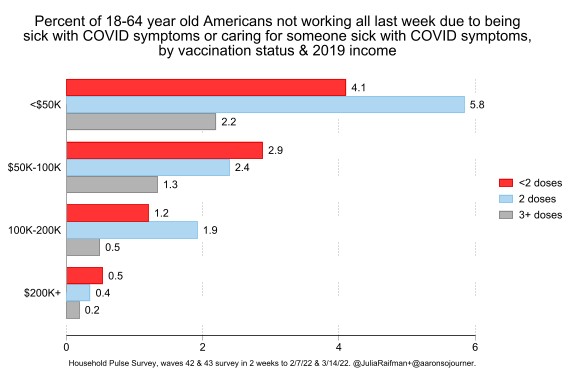
Increased risks of exposure for low-income people persisted despite vaccination status. While people who were boosted were less likely to report missing work in February and March of 2022, income disparities in missed work persisted even among vaccinated people, highlighting the role of exposure even among those who were vaccinated and boosted. For example, people who earned less than $50,000 and were boosted were more likely to report missed work than people who earned more than $200,000 and were not vaccinated.
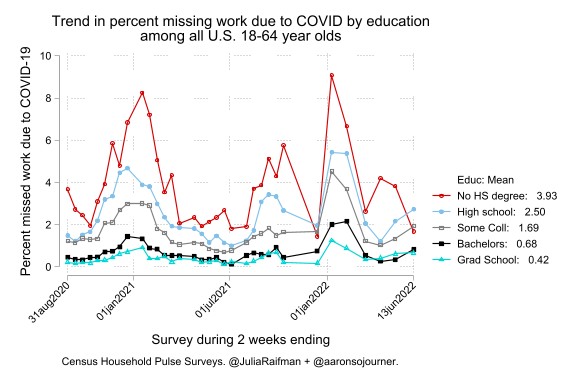
Education level also matters for who missed work. Americans who did not complete high school were about nine times more likely to miss a week of work due to dealing with COVID symptoms than Americans with a graduate degree, such as a law degree, master’s degree, or PhD.
Expanding the definition of persons at “high risk” will make policies more responsive.
While our current definition of populations at “high risk” includes people with an elevated risk of severe illness if infected—such as the elderly and immunocompromised—people at high risk of exposure who suffer worse health and socioeconomic consequences have largely been excluded. As a result, Black, Hispanic, Native American, and low-income Americans have systematically been deprioritized and excluded from policy provisions such as additional booster shots, antiviral treatments, and other medical care prioritization meant to protect high-risk individuals.
Our analyses, and prior analyses showing elevated death rates in lower-income counties, underline the importance of expanding the definition of high-risk populations to include these communities. Identifying populations at high risk of COVID is important for establishing policies and programs to reduce risk. In addition, recognizing low-income workers and Black, Hispanic, and Native American people at high risk of exposure conveys the importance of ensuring vaccinations, boosters, masks, and tests reach these populations.
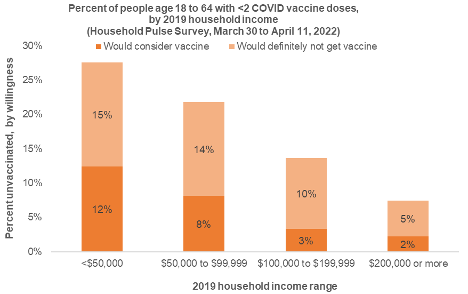
Despite the elevated risk of exposure to the virus, workers with lower household incomes in 2019 were less likely to report receiving at least two doses of the COVID-19 vaccine and more likely to report that they would be willing to consider getting vaccinated. Among the 27 percent of lowest-income HPS respondents who remain unvaccinated, almost half (44 percent) reported that they would consider vaccinating. In contrast, only 7 percent of Americans with incomes over $200,000 remain unvaccinated and have almost all achieved their preferred vaccination status. Building public health infrastructure for routine, direct vaccine delivery to low-income neighborhoods and workplaces could support more equitable vaccination rates and boosting.
Adopting an equity lens is essential to offset disparities in levels of exposure and the impacts of falling sick.
Evidence-based COVID mitigation policies, including vaccine and booster mandates and data-driven mask policies, reduce the disproportionately larger levels of exposure and severe disease faced by low-income, Black, Hispanic, and Native American community members. Unfortunately, the rapid rollback of public health measures increases their exposure rates. In addition to policies to reduce transmission and severe disease, congressional funding for vaccines, tests, masks, and ventilation is also key, especially for the 28 million uninsured Americans who cannot access these services for free. Further, an extension of the federal state of emergency beyond July 2022 is necessary for the continuation of free provisions.
Improving workplace protections through an Occupational Health and Safety Administration (OSHA) issued emergency temporary standard (ETS) could ensure workers at the highest risk of exposure are vaccinated, boosted, and have access to high-quality masks and tests. Preparedness to alert the population about more virulent novel variants and implement policies to reduce transmission are also especially important for populations disproportionately affected by COVID-19.
The current COVID-19 policy paradigm has not adequately addressed the precarity faced by low-income communities and communities of color. In addition to reducing potential exposure levels, policy should also address the disproportionate economic and health costs of falling sick that these communities face. Absent paid leave, infectious workers must choose between food for their family or the health of their customers and coworkers. Ensuring paid leave provisions for the lowest-income workers, including part-time or independent contractors, can help reduce food insufficiency and economic hardship caused by missed work due to COVID-19.
The continuation of COVID-19 safety policies and programs, including mailing tests to households and financial and social support programs, would reduce levels of exposure as well as the health and economic consequences of COVID-19. Reducing COVID-19 transmission would also reduce population-wide surge harms such as overloaded hospitals and service disruptions, and would reduce disparities. It is important to note that unlike most of their wealthy and white counterparts, people from marginalized communities lack the freedom to choose their level of exposure and the resources to ensure high standards of care. We therefore need targeted policies to provide a standard of safety for all.