Investing in Care: Exploring an Industrial Strategy for Care Work
May 23, 2024
By Suzanne Kahn
Introduction
As the Biden administration’s first term draws to a close, the care agenda remains one gaping piece of unfinished business. The administration’s original Build Back Better proposal included investments to provide universal preschool for three- and four-year-olds, reduce costs and expand access to childcare for younger children, and expand access to home care services for seniors and people with disabilities. All of these were left on the cutting room floor during negotiations over the Inflation Reduction Act (IRA) (White House n.d.).
In the year and a half since the passage of the IRA, much of the conversation about care policy has been around how federal investments in care work can bolster the industrial policies at the center of the IRA, the CHIPS and Science Act, and the Infrastructure Investment and Jobs Act. Care advocates, employers, and policymakers have all pointed out that care is as essential to a functioning and expanding workforce as roads and bridges; both allow workers to participate in the market (Zhavoronkova and Coffey 2023; Poo 2022). In response, the Commerce Department required that companies receiving CHIPS funds have a plan to provide childcare to all their workers (White House 2023). As welcome as this sort of innovation is, it is not a stand-in for the comprehensive investments in the care industries that are still required.
This brief offers an approach for thinking about care investments the next time there is an opportunity for major care legislation. Building on prior work by Roosevelt authors, this brief argues for an industrial strategy—defined as “any policy that encourages resources to shift from one industry to another”—for the care sector (Estevez 2023; Tucker and Sterling 2021). Moreover, it proposes a progressive approach to industrial care strategy, insisting that the government not only foster the growth of care industries but do so in ways that advance progressive social and economic goals. After digging into why this approach is necessary for our economy, this brief examines the many existing levers available for a consciously structured industrial strategy for care, including some that both federal and state governments experimented with during the COVID-19 pandemic. This brief ends by considering the best form of industrial strategy intervention given the specific challenges of the care industries, as well as what standards and guardrails need to be in place on such policies.

As a society and country, we desperately need care industries, but markets alone are not providing sufficient access to them. An affirmative industrial strategy of care would both strengthen our economy and democracy overall and serve as a vital complement to the other investments.
Care workers—childcare workers, home health aides, and others providing direct care for the most vulnerable in our society—make up roughly 17 percent of the US workforce (Wedenoja 2023). But these 24.1 million paid workers do not include unpaid care workers who have either stepped out of the paid labor force or reduced their paid hours to provide care for free to relatives and friends (Wedenoja 2023). The Boston Consulting Group estimates that the entirety of the US care economy, paid and unpaid, is up to $6 trillion (Kos, DasGupta, et al. 2022).
This sizable and growing sector of the economy must be understood as a set of vital industries that the government can and should foster—a sector that requires an industrial policy of its own.
While recent industrial strategy investments have neglected care, market-shaping federal investments in care industries are far from novel. As noted in previous Roosevelt reports, even at moments when the US has understood itself as not practicing industrial policy, the government’s policy decisions were actively shaping markets (Tucker and Sterling 2021; Hughes and Spiegler 2023). Arguably, the tax code and Social Security system have long shaped the care industries by encouraging the private and unpaid provision of care by giving favored tax status to single-earner families (Kessler-Harris 2003). As this policy has failed to keep up with rising costs of living over the last half century, and more and more families have moved to having all adults in wage-earning roles, the formal, paid care industries have expanded. This expansion is predicted to continue. The number of people working in the care economy is expected to grow by 10.5 percent over the next decade, almost twice the growth rate across all occupations (Wedenoja 2022).
As care work has become increasingly professionalized, we’ve also seen the rise of care sector unions (as well as the National Domestic Workers Alliance) as powerful forces for what should be understood as state-level industrial policies for care. For example, in the 2000s, SEIU 1199 set up close partnerships with hospital and health-care systems to lobby states and the federal government to expand Medicaid coverage in ways that have shaped and grown the markets for care work (Fink and Greenberg 2009). Likewise, 11 states collectively bargain with unions of home-based childcare workers, creating a system for the establishment of active industrial policies to grow and stabilize the home childcare sector (Collins and Gomez 2023).
Recent state and local-led efforts to expand access to public pre-kindergarten should also be understood as progressive industrial policy. In a recent paper, Josh Wallack (2023) shows how the build-out of 50,000 public, full-day pre-K seats in two years (2013–2015) in New York City required a robust industrial strategy that vastly expanded the industry and set new standards for workers within it.
In short, in the first decades of the 21st century, we have seen increasingly deliberate attempts at state-level industrial strategies for the care economy. It’s time for the federal government to embrace this policy practice as well. But deliberate industrial strategy is not one-size-fits-all. Saying we need a national, industrial strategy for care is only the start of the conversation about which of the many industrial policy tools at the government’s disposal would best shape care industries. This brief offers not only the case for an industrial strategy for care but a guide for how to think about additional questions that such an approach to care will inevitably surface. For example, are industrial policy investments in care best funneled through the private sector, or should we consider direct public provisioning in some cases? And, as another example, when public money does flow to private corporations, what guardrails should be attached?
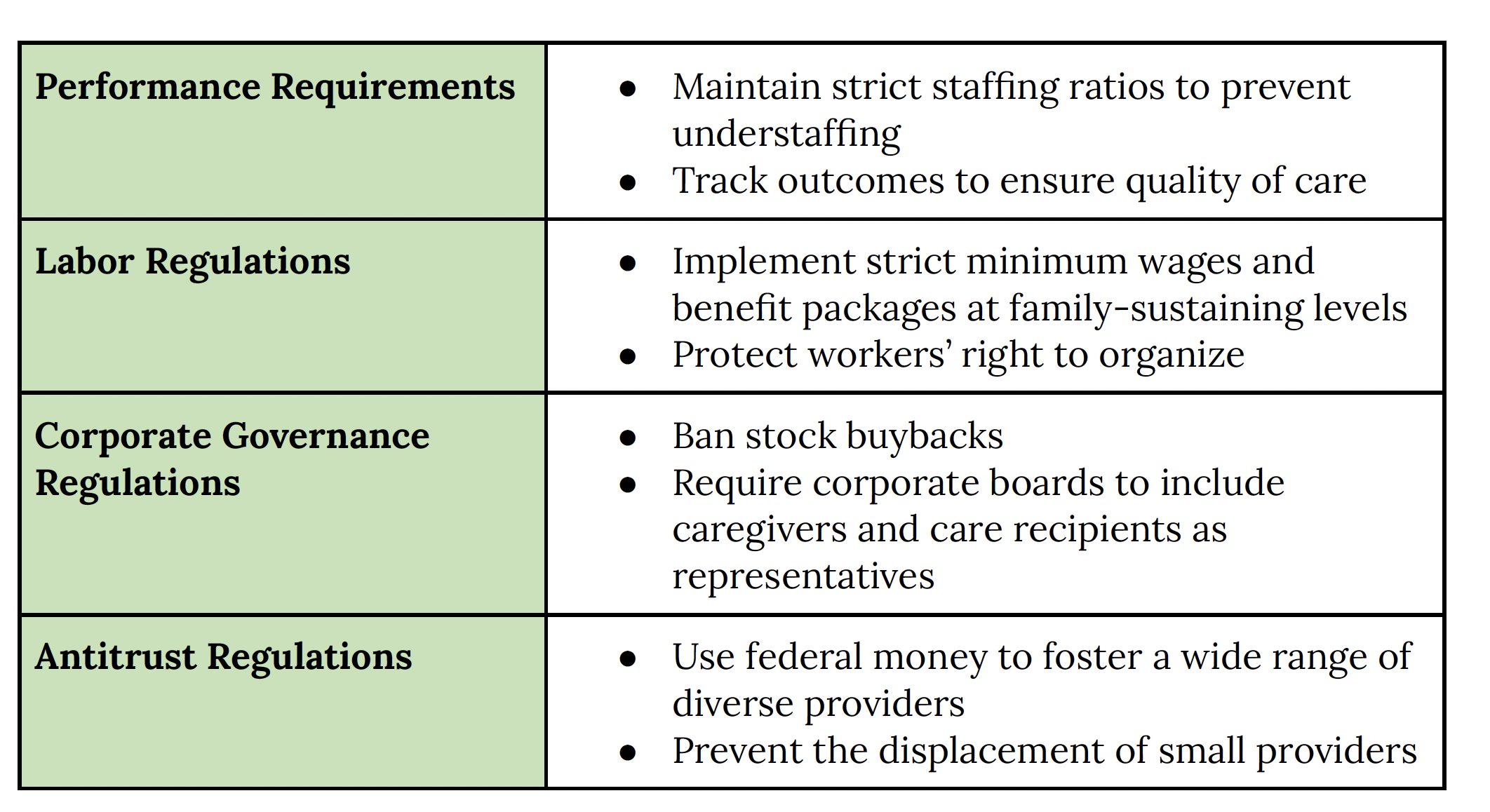
Standards and Guardrails Crucial to Equitably Investing in the Care Industry
A conscious industrial policy requires attention not only to investment but also to the standards and guardrails put on those investments. We will not solve our care crisis over the long term if new public spending gets funneled to and extracted by for-profit corporations. We need to not only use public funds to expand these markets but do so in a way that crafts these markets to be more equitable. Some standards and guardrails that will be particularly important in the care industries are strict performance, labor, corporate governance, and antitrust regulations.
Levers for an Industrial Policy of Care
The government’s current involvement in care markets means that there are many existing levers available for structuring a robust industrial policy of care. At the same time, that involvement is significantly less than what it should be even in comparison to similarly situated countries. This brief examines where those existing levers might be deployed given existing government involvement in the care industries.

New Money
While the United States famously spends significantly more on health care than other OECD countries, the same cannot be said for long-term care or childcare spending (OECD 2022). When it comes to spending on early childcare, the US is a famous outlier among OECD countries, spending only a small fraction of what similarly situated countries do on childcare on a per-capita basis (Miller 2021). Our spending on long-term care is not quite so bleak, but still hovers around the OECD average and well below that of the UK, France, and Germany, for example (OECD 2020). We are also one of the only developed countries that does not offer some version of universal long-term care benefits (Sammon 2020).

Medicare/Medicaid
The vast majority of spending on home health care (care provided in the home related to a specific health need, with the aim of recovery) and long-term care (care for individuals who need ongoing assistance because of age, disability, or illness) is paid for through Medicaid and other public programs. Seventy-one percent of home health care is paid for by public programs (Zhang 2023), and over 72 percent of long-term care services are paid for by public funds (Colello and Sorenson 2023). As a result, almost all home care workers receive at least some of their paycheck from public sources. This means that even if we don’t conceptualize it this way, these programs are already setting industrial policies for the care industries.
Private Insurance
Medicaid and Medicare pay for such a large share of the long-term care and home care industries because we lack both public options for long-term care and a working private long-term care insurance market. As a result, the primary existing levers for executing an industrial policy in these industries are Medicaid and Medicare, but it’s worth considering how the private insurance market, such as it is, also creates points of entry.

Childcare
In 1971, the United States almost created a national system of federally funded public childcare centers across the country, but President Nixon vetoed the bill, explicitly stating that he believed childcare should be handled by family and community (Waxman 2021). Since 1971, a patchwork system of subsidies has grown, giving the federal government only a small amount of leverage within the system (US Department of HHS Office of Child Care 2014). In comparison to the well-over two-thirds of the national long-term care budget covered by public spending, only about one-third of childcare spending comes from the federal government (US Department of the Treasury 2021).

State-Level Levers
To the extent that the federal government has built out its public care infrastructure in the US, this has overwhelmingly been through means-tested programs aimed at the lowest-income people. As a result, states actually hold a large share of the existing leverage in care policy. Historically, means-tested programs designed for the least advantaged have been more likely to be organized as federal-state partnerships, while broader, more universal programs have been organized at the federal level. In large part, this is the legacy of racist governing compromises that allowed southern states to manage and thereby exclude Black people from social safety net programs (Katznelson 2023).
